Watch the welcome video to learn about your plan
Watch the welcome video to learn about your plan
Get to know some of the features and resources available through your plan.
Welcome to your Aetna Dual Eligible Special Needs Plan, or D-SNP!
Our number one goal: making it easy to get the care you need. And we start right away with a welcome call from a member of our team.
During the call, we will:
- Confirm your plan selection
- Review your primary care provider, or PCP, and other doctors
- Discuss your pharmacy and prescriptions
- And explain your covered services and added benefits.
With your D-SNP, you get medical and prescription drug coverage, including $0 copays on covered Part D prescriptions at in-network pharmacies, plus dental, vision and hearing coverage and more.
You’ll get a verification letter and e-notice about your plan. In it, you’ll learn about these and other D-SNP benefits as well as the allowances you get for dental, vision and hearing. Be sure to review this important plan information.
You will also receive your Aetna member ID card in the mail. Your PCP will be printed on your ID card. Our plans require you to have a PCP. If you didn’t choose a PCP when you enrolled, one was assigned to you.
Need to change your PCP? Call Member Services at 1-866-409-1221 (TTY: 711) between 8 AM and 8 PM local time, Monday through Friday. They can help you find a new one.
Always bring your Aetna member ID card with you to pharmacies and doctor visits, along with your Medicaid ID card if you have one.
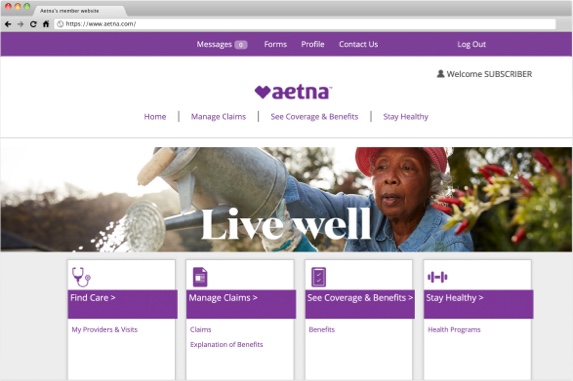
You can also see your ID card online when you register for a secure account at AetnaMedicare.com/MyDSNP.
It’s easy to register, and you can log in at any time to find network providers, schedule a flu vaccine, view your prescriptions and claims and more.
All Aetna® D-SNP plans also come with an Extra Benefits Card, a Benefits Mastercard® Prepaid Card, to help pay for certain everyday expenses.
As a new D-SNP member, you will receive your Extra Benefits Card in the mail before or shortly after your plan starts, along with important information, including:
- Your card spending Wallets
- Your monthly allowance amounts
- How to activate your card
- How the card works
- Where you can use the card
- And what you can pay for with your card, including healthy foods and select over-the-counter items.
As an Aetna® D-SNP member, you also have a personal care team. They make it easier to get the care you need. A member of your care team will call you after your plan starts.
Together, you’ll complete a health survey to get to know your needs, create a care plan with your doctors and help you get the right care and programs.
You can also complete the survey on your own on your computer or smartphone. Go to AetnaMedicare.com/MyHealthSurvey to get started.
They can help you schedule doctor visits and may even be able to help you set up a ride. And they can connect you with local programs for finding healthy foods, safe housing and more. You can reach out to your care team with any questions about your health.
Have a health question after hours? No problem. You can call the 24/7 Nurse Line at 1-866-409-1221 (TTY: 711) for answers anytime, including nights and weekends. The Nurse Line number is also listed on your member ID card.
If you have any questions about your plan benefits and how they work, your dedicated Member Services team is here to help. You can reach them at 1-866-409-1221 (TTY: 711) between 8 AM and 8 PM local time, 7 days a week.
You can also find helpful information and plan documents at the member website: AetnaMedicare.com/MyDSNP.
We look forward to helping you get the care you need.
Helpful resources
Search providers and prescription drugs
It’s always a good idea to find out what is and isn’t covered by your plan. Use the links below to search for specific doctors and medicines.
The Aetna Extra Benefits Card can help with certain everyday expenses
Aetna® Dual Eligible Special Needs Plans, or D-SNPs, give you an Aetna Medicare Extra Benefits Card to help pay for everyday expenses like healthy foods, over-the-counter health products and even rent.
That’s on top of our medical coverage and $0 copay for covered Part D prescriptions at in-network pharmacies. Plus, we offer D-SNPs with dental, vision and hearing benefits.
We make it easy, too. If you’re a new member, we’ll mail you an Extra Benefits Card, a Benefits Mastercard® Prepaid Card, with monthly allowances called “Wallets.”
If you’re a returning member, you can continue to use the Extra Benefits Card you already have — be sure to hold on to it. You’ll receive a letter from NationsBenefits explaining your card changes and new Wallets.
All D-SNP members get Wallets they can use to buy healthy foods like fruits and veggies, meat and seafood, healthy grains like bread and pasta and pantry staples like flour and spices.
You can also buy select over-the-counter, or OTC, health and wellness items, like pain relievers, cold and flu medications and first aid supplies.
The Extra Supports Wallet is our most flexible allowance. It can be used to help pay for healthy foods and OTC items along with several other approved products and services, including:
- Rent or mortgage assistance
- Personal care items
- Utilities
- Transportation
- And pet care items
Wallets vary by plan. Check coverage in your area.
Your Extra Benefits Card will come with information on how and where you can use your card as well as your Wallet amounts.
To use your card, you’ll need to activate it. You can do that three ways.
1. Phone. Call 1-877-204-1817 (TTY: 711) to speak with a Member Experience Advisor. The number is also on your Extra Benefits Card.
2. QR code. Simply scan the QR code in your Extra Benefits Card welcome materials.
3. Online. Go to Aetna.NationsBenefits.com/Activate
Once your card is activated, your funds are available to spend. You can spend them however you like on any approved products or services.
Not sure if an item is approved for purchase? It’s easy to look up covered items using the NationsBenefits mobile app on your smartphone. The app is available for free on the App Store® and the Google Play™ store.
The Extra Benefits Card can be used at approved retail locations. At checkout, simply swipe your card and select credit when prompted for payment type. No PIN is required.
If your Extra Benefits allowance covers your full purchase, you’re good to go. You’ll need to use a different payment method if any of your items or services aren’t approved, or to pay for the remainder if you’ve used up your allowance. You can check your balance at any time on the NationsBenefits app.
Your Extra Benefits Card helps you put your health first so you can feel your best. To learn more, visit Aetna.NationsBenefits.com
The Aetna Extra Benefits Card can help with certain everyday expenses
Your Aetna D-SNP gives you an Aetna Extra Benefits Card to help you pay for certain everyday expenses. The Extra Benefits Card will be automatically loaded with your Wallet allowance amount(s) each month.
Watch the video to learn more.
The Aetna Extra Benefits Card can help with certain everyday expenses, like:*
Healthy foods
Select Over-the-counter (OTC) health and wellness items
Check your Evidence of Coverage (EOC) to see all of the ways you can use your Extra Benefits Card.
How your plan works
How your plan works
Take a moment to look over these useful resources with your caregiver or family members who help with your health care. These documents will explain the details of your plan, how it works and what’s covered.
Select below to view your:
- OTC catalog
- Evidence of coverage (EOC)
- Summary of benefits
- List of covered drugs (formulary)

It’s easy to get the care you need
These days, you can get medical care at many different places. You could go to your doctor’s office, a walk-in clinic, an urgent care center or the emergency room. But how do you know which one to choose when you’re hurt or feeling sick, or when you need a vaccination? These tips can help you make the right care decision in the moment.
Your primary care provider, or PCP, should always be your first choice for any non-emergencies. Your PCP knows your medical history. They can help you manage common illnesses like the flu and chronic conditions like diabetes. They can also prescribe medications and refer you to a specialist if needed.
Can’t get an appointment with your PCP? In that case, a walk-in clinic like a CVS MinuteClinic is a good choice for convenient and affordable care. You'll likely see a nurse practitioner or physician’s assistant.
They can help treat rashes and minor injuries and diagnose common illnesses like colds and flu. They can also do routine tests like blood pressure, blood sugar, A1C and cholesterol checks. And they can give immunizations (like a COVID-19 or flu vaccine) and prescribe or refill medications.
While walk-in clinics don’t require appointments, they do operate on a first-come, first-served basis. So you may have to wait to be seen. Many walk-in clinics are also in or near a pharmacy. That makes picking up your medications easy. Can’t get to a clinic? You can make an appointment for a virtual visit at a MinuteClinic E-Clinic.
If your health issue is more serious, you may want to go to an urgent care center. They have doctors on staff who can treat you for issues such as broken bones, cuts that need stitches, nausea, vomiting, diarrhea, rashes and fever. Most urgent care centers can also do X-rays and get some test results while you wait.
Finally, head to the emergency room right away if you have a medical situation that needs immediate attention. This includes chest pain, difficulty breathing, sudden changes in mental ability, slurred speech, uncontrollable bleeding, head injuries, sudden loss of vision or seizures.
If your situation is life-threatening or you’re alone and can't drive yourself to the ER, call 911. This is especially important if you’re having chest pain or symptoms of a stroke. A paramedic can begin treatment right away, which could save your life.
Still not sure where to go? As an Aetna Dual Eligible Special Needs Plan, or D-SNP, member, you can call your care team for direction. They may also be able to arrange transportation to the right location. If your care team isn’t available, you can call the 24/7 nurse line for round-the-clock health guidance.
Knowing where to go for medical care can help you get the proper treatment, and possibly save you time and money too. Wherever you go, remember to bring your Aetna member ID card with you.
To learn more ways your Aetna D-SNP plan can help you get the care you need, visit AetnaMedicare.com/MyDSNP
It’s easy to get the care you need
Your plan has you covered
If you’re suddenly sick or injured, you may think you should go to the emergency room (ER). But, depending on your medical issue, the ER may not be the best choice. Telehealth and retail clinics like MinuteClinic® locations can be a more convenient way to get quick care. If you’re not sure where to go, you can call the Aetna 24/7 Nurse Line for help.
Help for caregivers
Help for caregivers
Being a caregiver can be hard. We understand that. And we want to help make what you do a little easier. That’s why we’ve created some helpful tools especially for caregivers:
Caregiver Information release form

Your monthly member newsletter

Your monthly member newsletter
Stay up to date with your monthly member newsletter, wellness & you.
Get the latest news about your benefits. See tips to help you on your journey to better health. You can quickly view the latest editions right here:
Latest Edition:
Past Editions:
Get in touch with your care team today
1-866-409-1221 ${tty}
${hours}
Disclaimer
*FOR EXTRA BENEFITS CARD EXPENSES: Benefits available on card vary by plan.
See Evidence of Coverage for a complete description of plan benefits, exclusions, limitations and conditions of coverage. Plan features and availability may vary by service area. The formulary may change at any time. You will receive notice when necessary.
Aetna and MinuteClinic, LLC (which either operates or provides certain management support services to MinuteClinic-branded walk-in clinics) are part of the CVS Health® family of companies.
The benefits mentioned are a part of special supplemental program for the chronically ill. Not all members qualify.
If your plan’s Extra Benefits Card includes rollover, any unused amount will rollover into the next month. The month amount can be rolled over through the end of the plan year but will not carry over into the next plan year. Eligibility for the Model Benefit or Reward and Incentive (RI) Programs under the Value-Based Insurance Design (VBID) Model is not assured and will be determined by Aetna after enrollment, based on relevant criteria (e.g., clinical diagnoses, eligibility criteria, participation in a disease state management program).